‹ Left atrial structures and differential diagnosis
Remnants

a
b
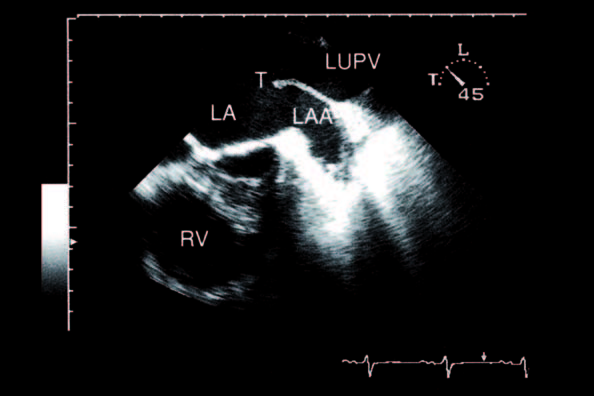
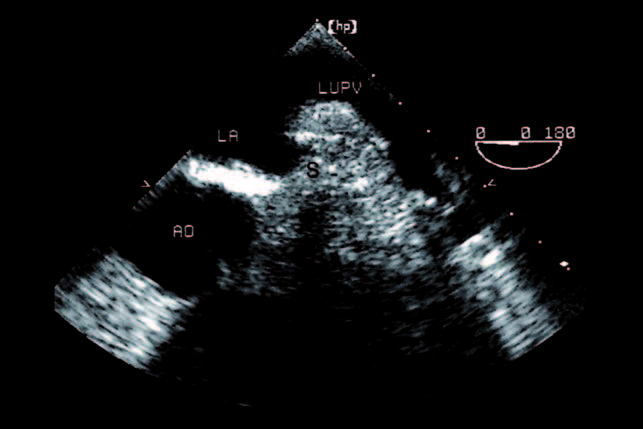
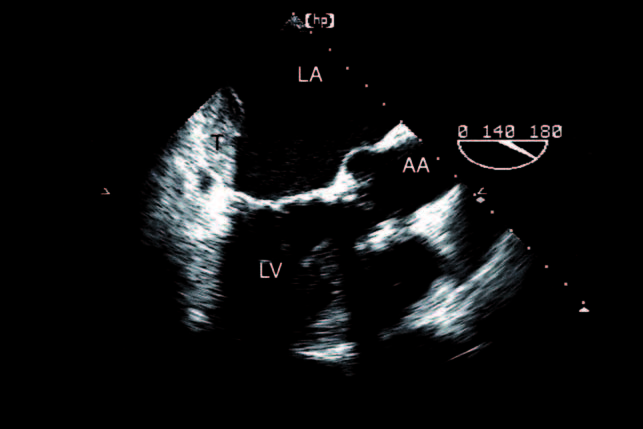
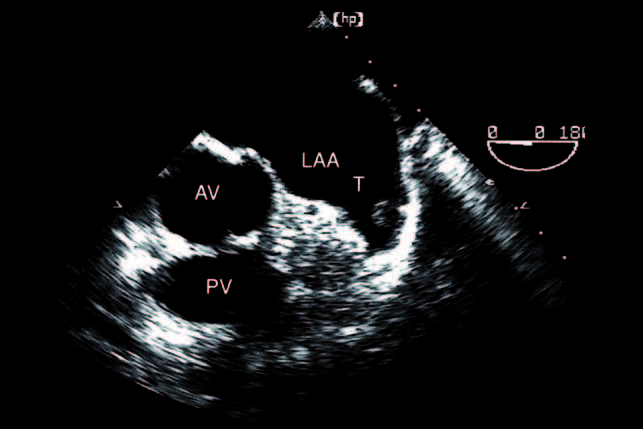
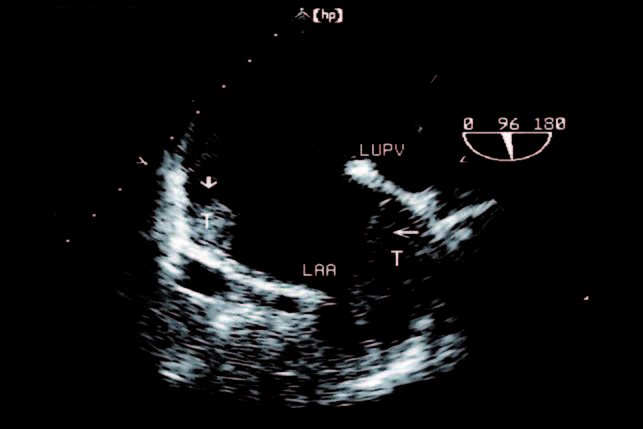
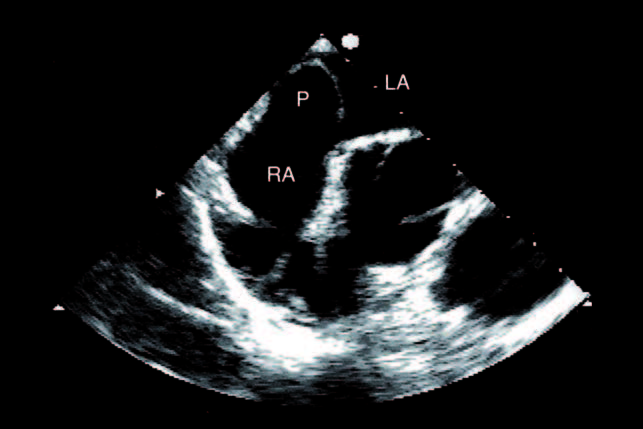
Between the orifice of the left upper pulmonary vein and the left atrial appendage, note the masslike tissue (remnant) which should not be interpreted as a tumour. It can be more or less infiltrated with fat. Sometimes this structure is called 'warfarin ridge' because this drug was occasionally mistakenly prescribed in patients with thromboembolic events (a, b).
Pectinate muscle
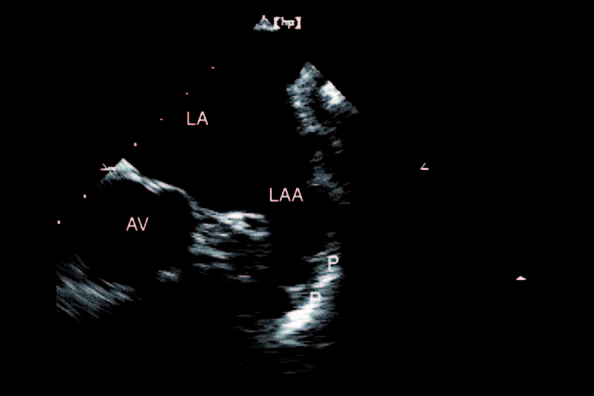
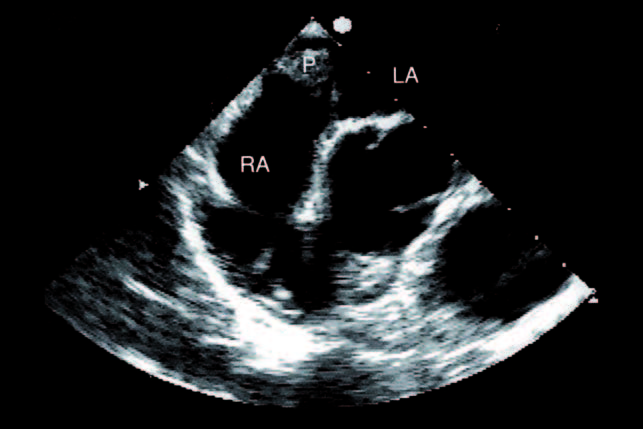
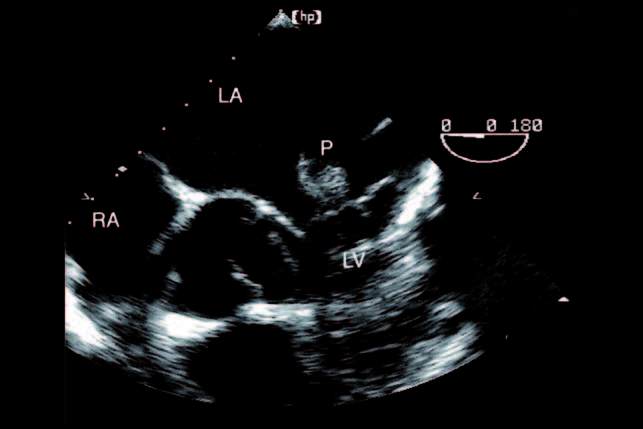
The picture illustrates the typical appearance of the pectinate muscle in the left atrial appendage that should not be misinterpreted as thrombi (P).
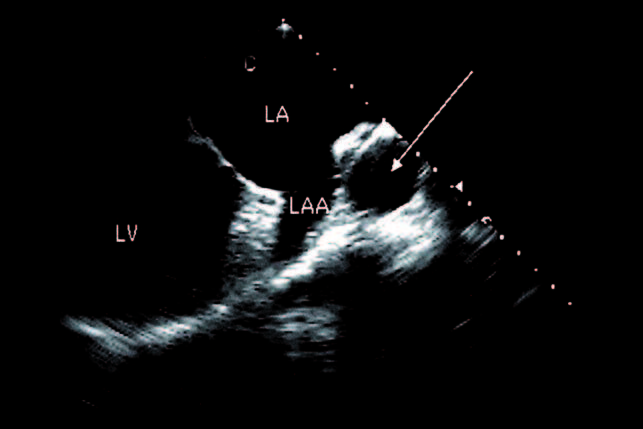
As depicted in this picture, the pectinate muscle need not be prominent. Remember the left pulmonary artery is a normal finding (arrow).
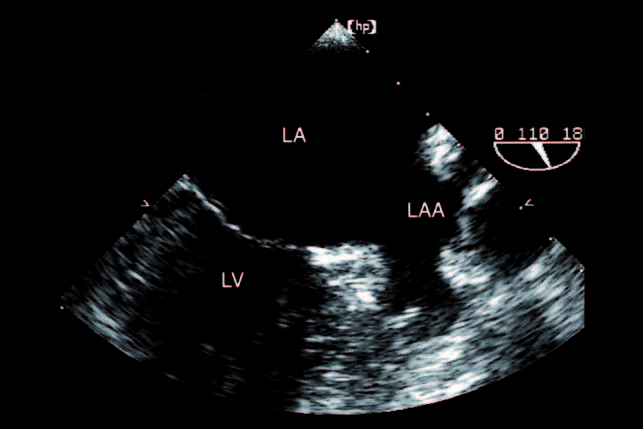
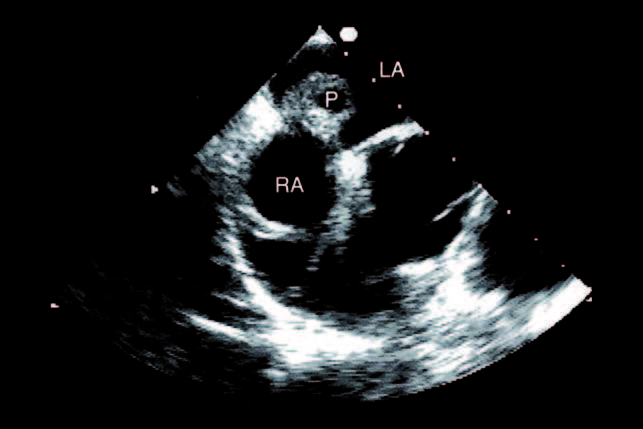
Variants of left atrial appendage. Left atrial appendage morphology can range from sharp to flat and lobulated. This picture is taken from a patient with lobulated left atrial appendage.
Be aware of shortening or inadequate visualization of the left atrial appendage when searching for thrombi.
Thrombi
a
b
Thrombi of left atrium. From transthoracic (a) and transoesophageal (b) approaches
a
b
In a patient with severe mitral stenosis, left atrial thrombi could only be detected with transoesophageal echocardiography (a, b).
Thrombi of left atrial appendage. Thrombi localized in the left atrial appendage can present as small (a) and large (b) round structures, as large pedunculated tumours (c), and as huge thrombus material as illustrated in a patient with almost complete filling of the left atrial appendage (d).
a
b

c
d
a
b
This patient, who had a mechanical valve prostheses, had interrupted anticoagulation therapy during his holidays. After two weeks of subsequent anticoagulation therapy, thrombi were substantially smaller without intermediate embolization (a) and after a further three months therapy only a small thrombus remained (b).
a
b
c
Thrombus through patent foramen ovale. Spontaneous echo contrast. Note the echodense (a), partially diffuse and circular structure of spontaneous echo contrast in the left atrium and atrial appendage without clear borders preceding thrombus formation. (d,e,f)
d
e

f
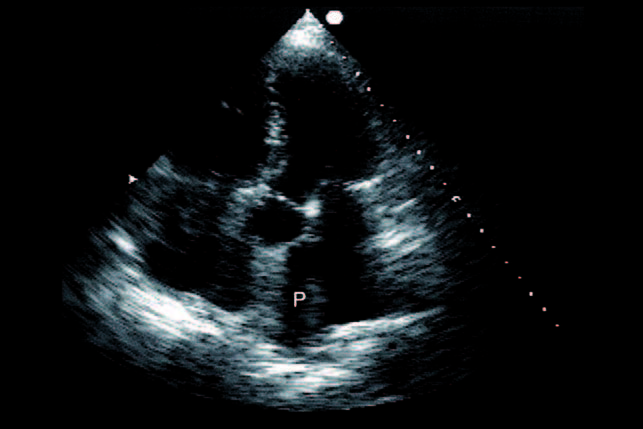
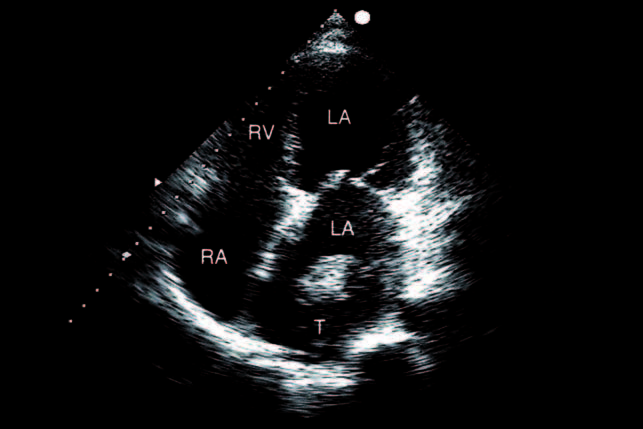
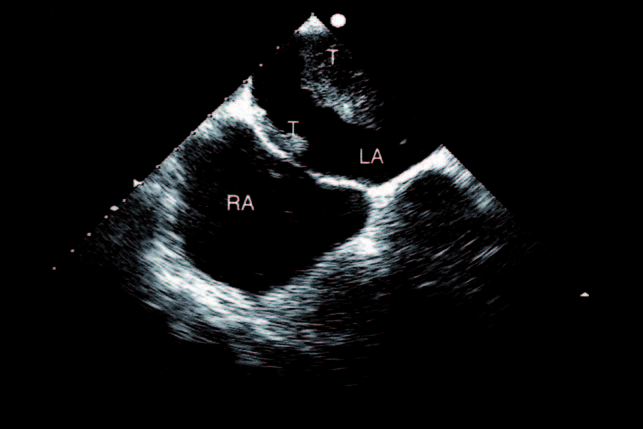
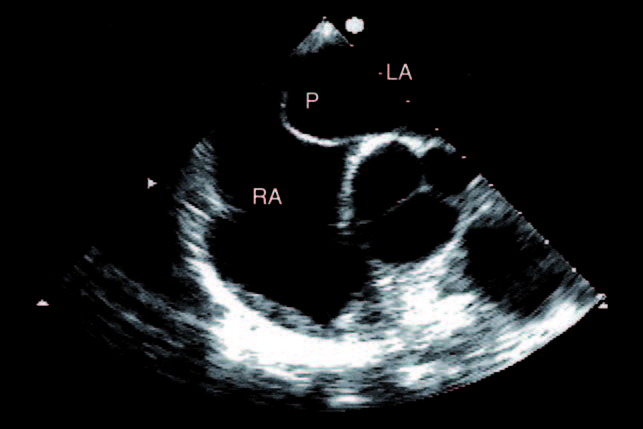
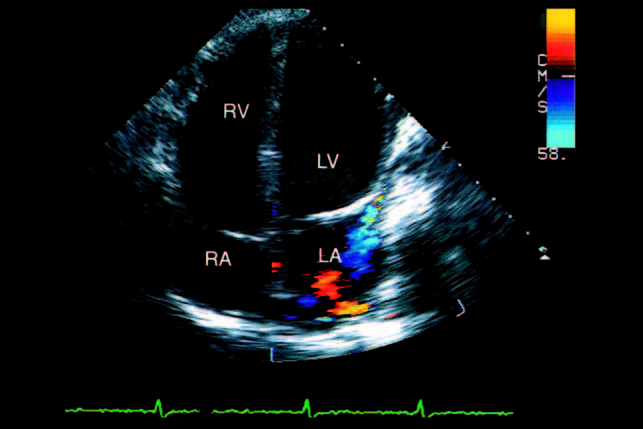
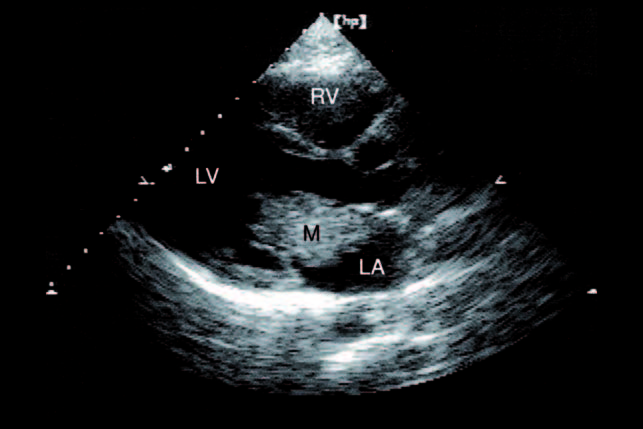
A proven artificial tumour from an inter-atrial septum in the left atrium is shown in a patient prior to surgery for pulmonary embolism. Note the dilated right ventricle with a septal bulge into the left ventricle due to elevated pulmonary artery pressure.
a

b
Note pseudo-thrombus of the mitral valve in the transoesophageal approach with documentation of a filiform tumour at the anterior mitral leaflet that can be unmasked as flail chordae of the mitral valve from another view (a, b).
a

b

c
Thrombi in the pulmonary veins. In a transplanted patient thrombi in the pulmonary vein arising from the insertion of the donor heart can be found. See examples from different views (a, b, c). Remember to distinguish this pathology from the similarly appearing metastasis of lung or vessel cancers entering the left atrium through the pulmonary veins.
a
b
c
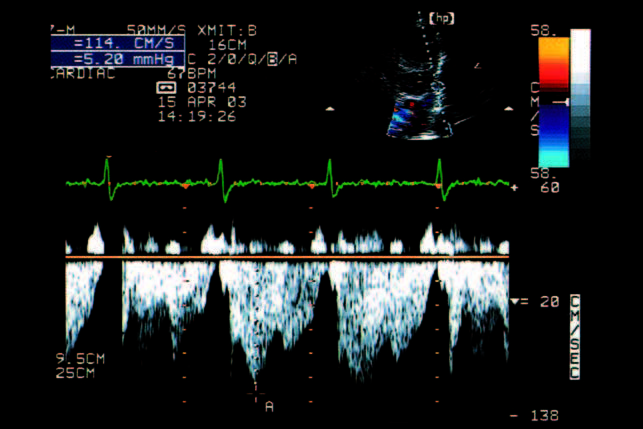
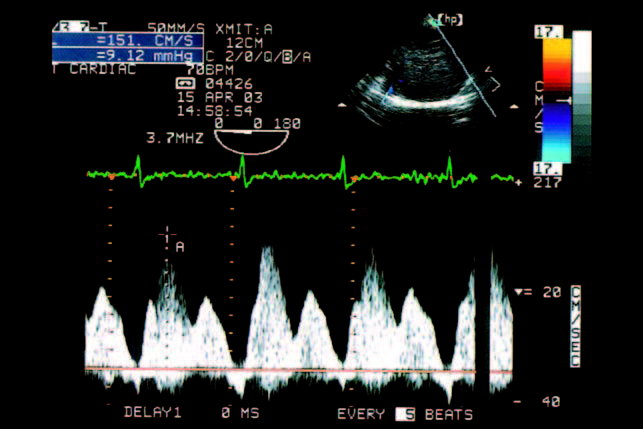
Pulmonary vein compression. Pulmonary veins can be compressed from extra-cardiac tumours. This is an example of a compressed pulmonary vein due to lung cancer in the apical five chamber view (a); the increased pulmonary vein flow of 114cm/sec in the PW-Doppler tracing from the transthoracic approach (b), and of 151 cm/sec from the transoesophageal approach (c) indicate stenosis.
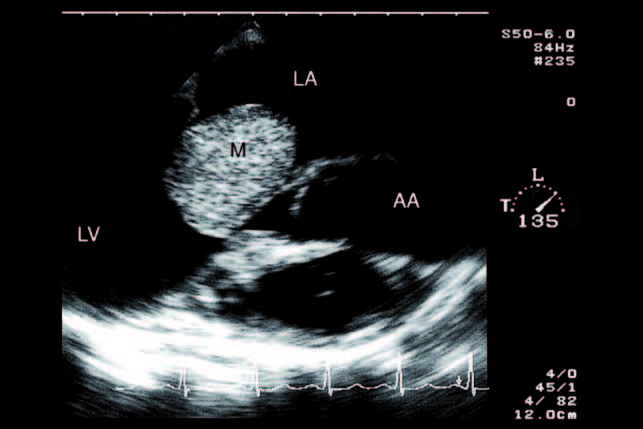
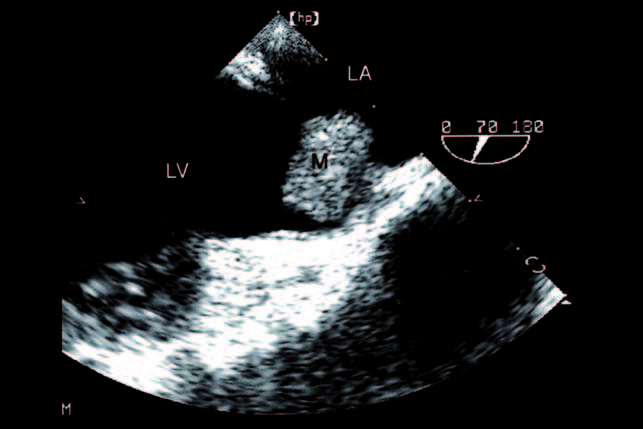
Myxoma
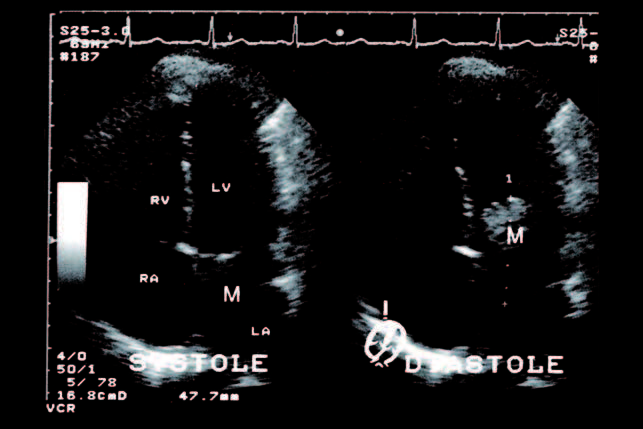
a
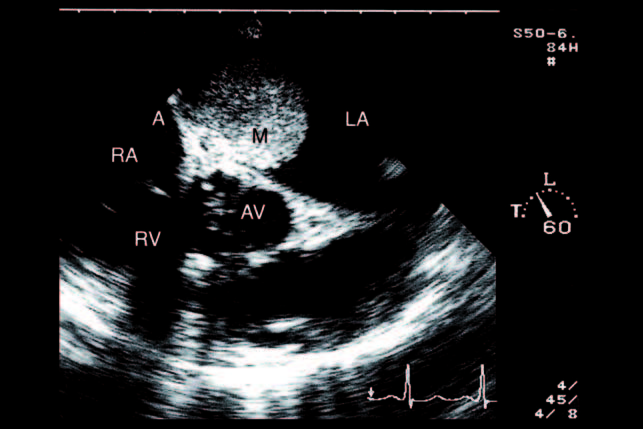
Myxoma can present with different morphology. One example shows a histologically proven echo-dense myxoma (48mm) with a smooth surface in the left atrium attached to the inter-atrial septum from TTE, and with nearly complete obliteration of the mitral annulus during diastole with a characteristically functional mitral stenosis (a).
b
The tumour, and especially the attachment site (large arrow), can be even better delineated from tissue Doppler imaging (b).
c
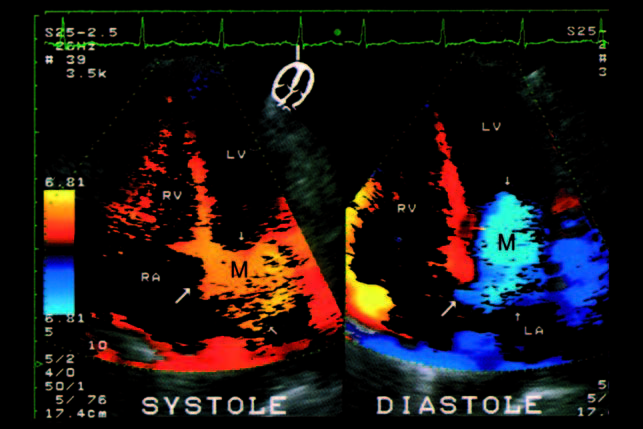
Picture (c) from the TEEapproach shows the attachment site at the inter-atrial septum, picture (d) the obstructed mitral annulus during diastole, and picture (e) the pseudo-mitral stenosis and the mitral insufficiency with colour Doppler echocardiography.
d
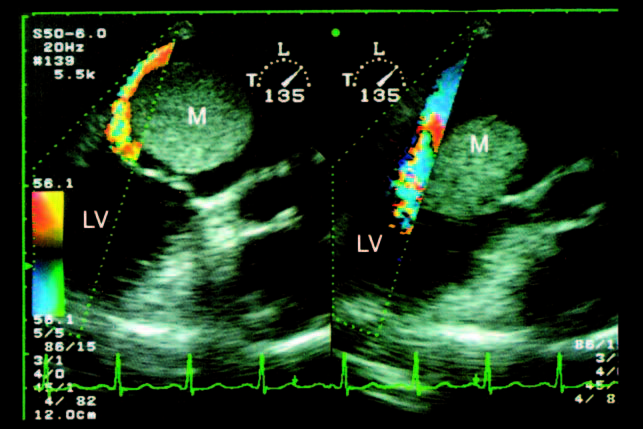
e
a
b
This example is taken from another histologically proven myxoma attached to the interatrial septum and shows an irregular surface on TTE (a) and TEE (b).
a
b
This example shows an nonhomogeneous immobile proven myxoma with a large attachment at the junction between the interatrial septum and the mitral annulus from TTE (a) and TEE (b).

This example is taken from a proven myxoma with embolic events and in the transoesophageal approach one can see the filiform surface of the tumour. Myxoma can also be infected with bacteria, which should be remembered when searching for vegetations.
a
b
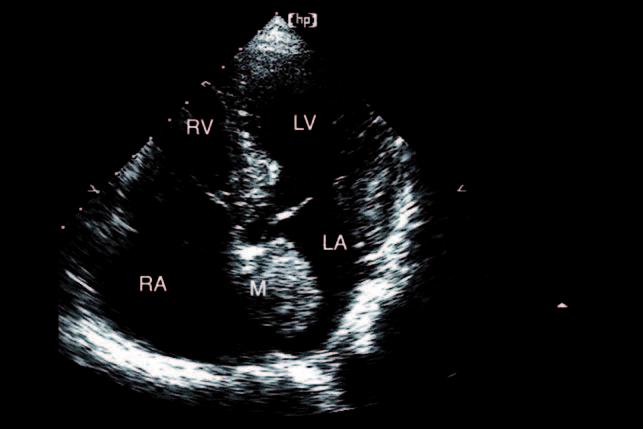
c
d
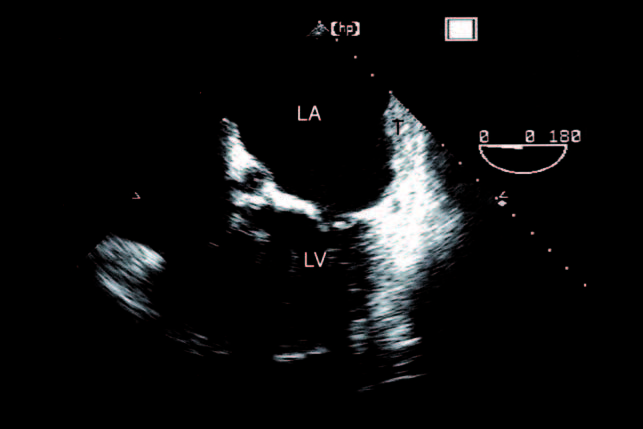
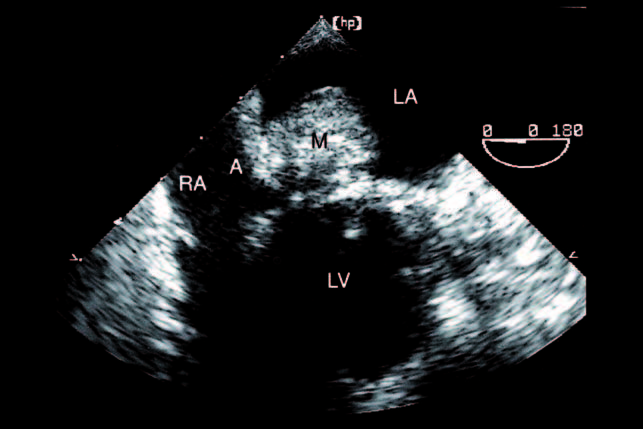
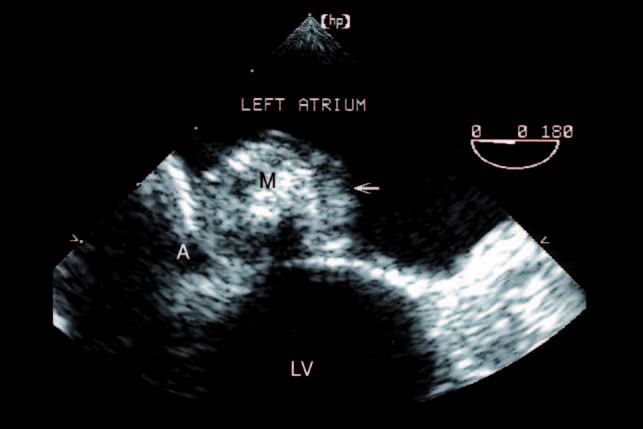
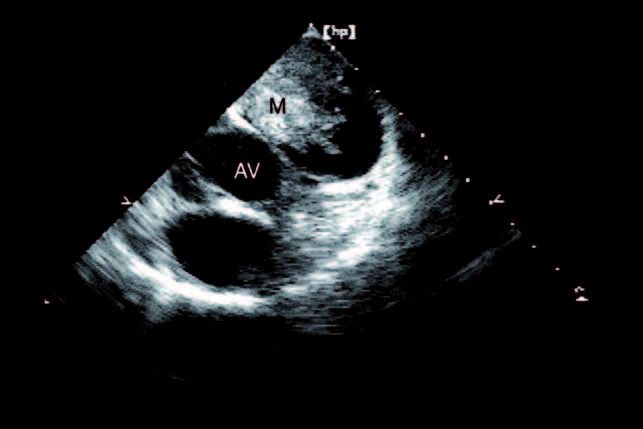
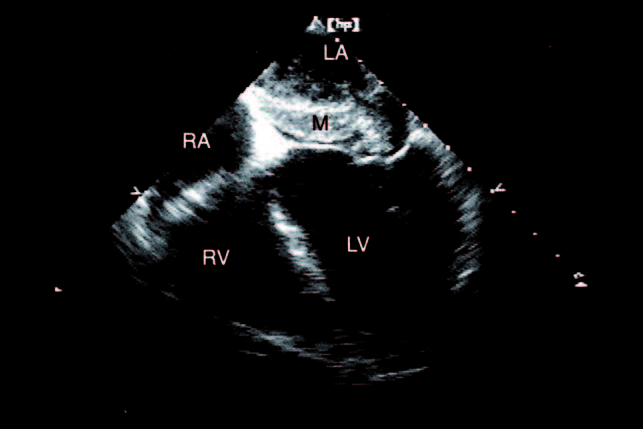
This example is taken from a histologically-and microbiologically-proven infected myxoma and shows the myxoma in the transthoracic long axis (a), apical four-chamber view (b), and from a transoesophageal approach (c, d).
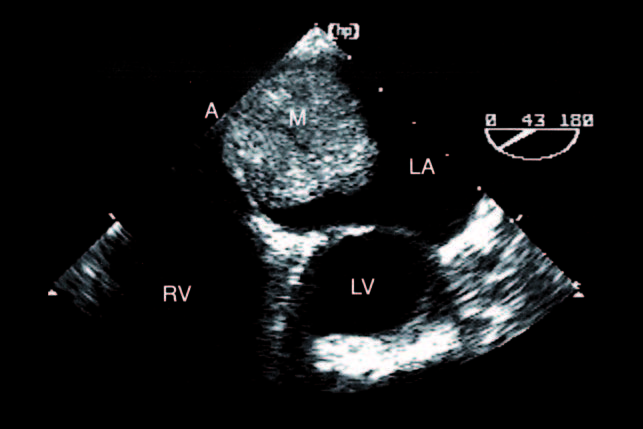
a
b
c
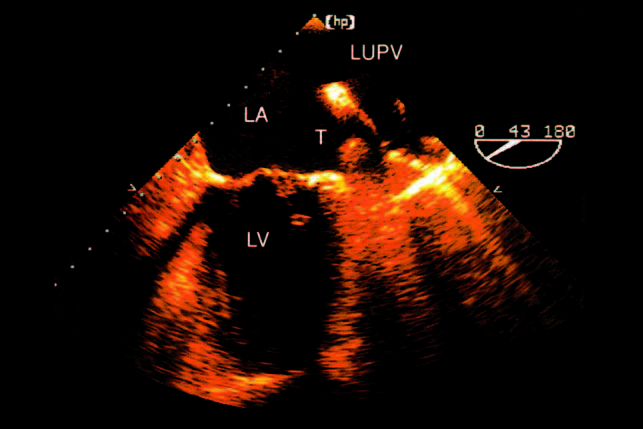
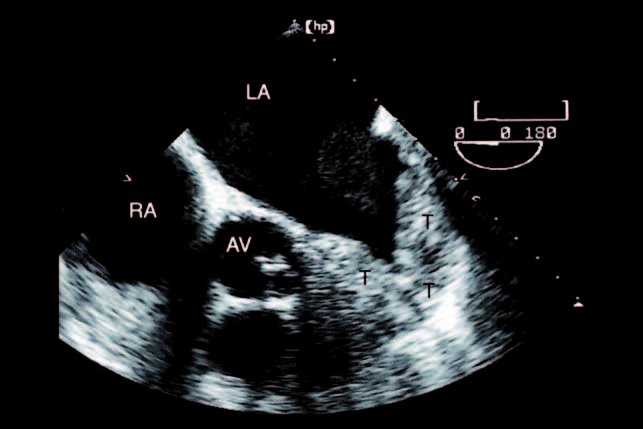
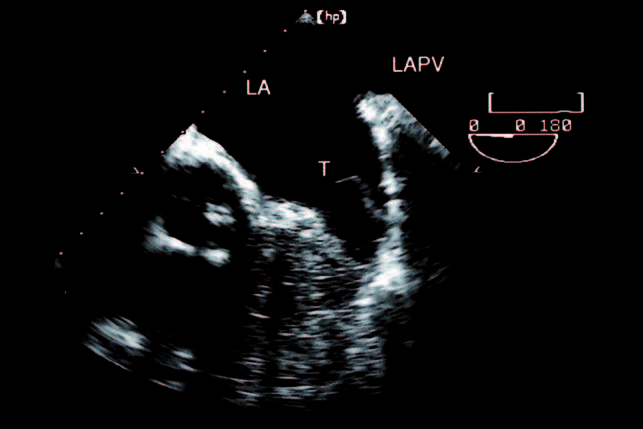
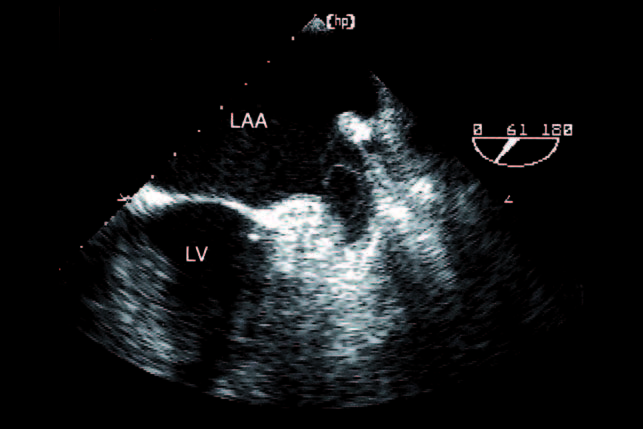
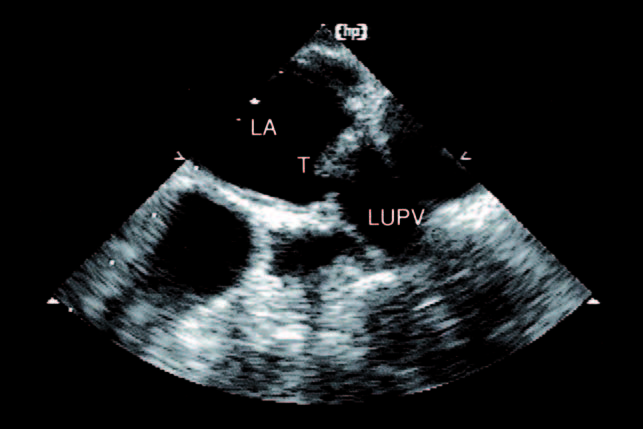
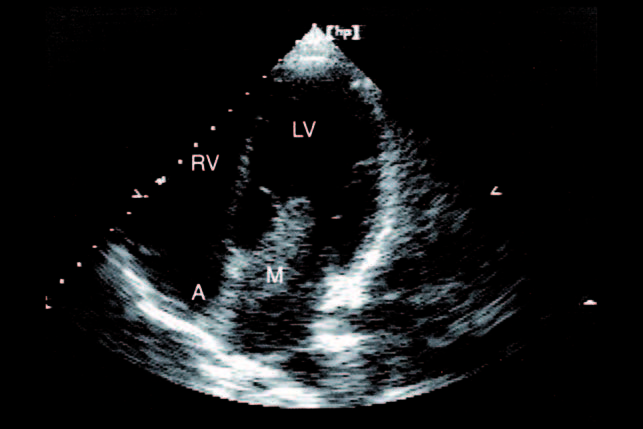
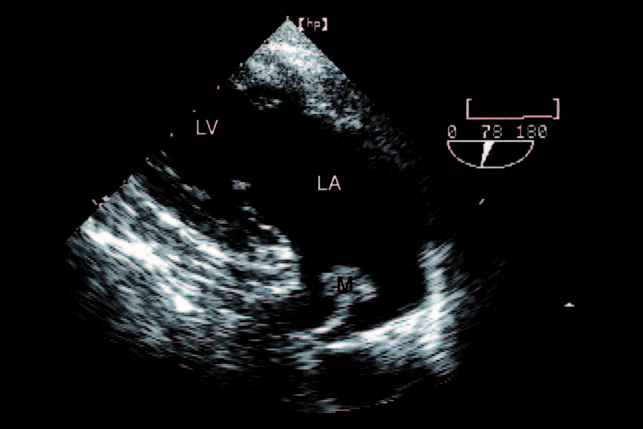
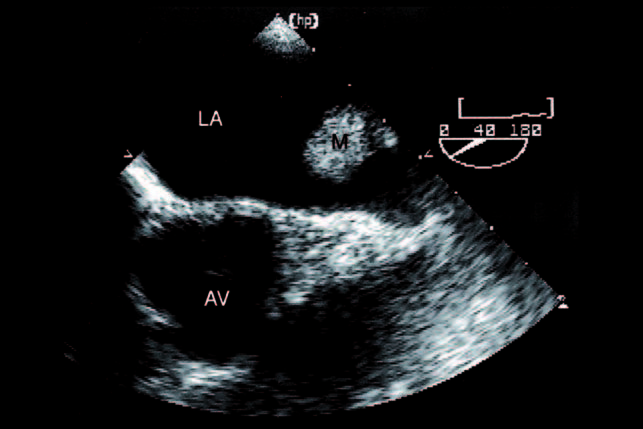
Myxoma found after embolic events can be small and might have atypical localization as in this example of a small proven myxoma between the entrance of the left upper pulmonary vein and the left atrial appendage, viewed from transgastric (a) and basal transoesophageal (b, c) approaches.

